
DCMS online
. org
Northeast Florida Medicine
Vol. 67, No. 1 2016
17
Palliative Care
Nausea and Vomiting
Nausea and vomiting are other causes for acute emer-
gency department visits in the palliative care population
and significantly affect quality of life. Identifying the eti-
ology andpotentially reversible conditions shouldfirst be
explored. Once initiating treatment, understanding the
cause of symptoms greatly influences any pharmacologic
intervention. Basic understanding of the emetic pathway
is vital in providing targeted therapy. Simply, the central
vomiting center receives input fromboth central (cortex,
vestibular, chemoreceptor trigger zone) and peripheral
afferentpathways.Emetogenicneurotransmitters include
dopamine, serotonin, histamine and acetylcholine.
7
Centrally, the chemoreceptor trigger zone (CTZ)
mediates the most frequent causes for nausea. Given its
location on the floor of the fourth ventricle, where the
blood brain barrier is porous, toxins, metabolites, and
drugs (opioids and chemotherapeutic agents) can be
highly provoking.The CTZ then stimulates the central
vomiting center via dopamine and serotonin. Initial
therapy targeting this area should be addressed using
dopamine antagonists (metoclopramide, prochlorper-
azine and haloperidol). Secondarily, ondansetron can
be added. In the palliative population, ondansertron
is generally reserved for intractable symptoms, save
those related to chemotherapy/opioid induced nausea
and vomiting.
7
Peripherally, GI tract causes of vomiting are me-
diated by both vagal and splanchnic afferents from
mechano/chemo receptors. Serotonin and dopamine
are the primary neurotransmitters involved.Typically,
a first line agent, after ruling out bowel obstruction, is
metoclopramide given its dual central and peripheral
actions on serotonin and dopamine. Prochlorperazine
and haloperidol are alternatives. Again, ondansetron
is a viable and safe option but effects are limited to
serotonin antagonism only.
Initiate therapy with attempts to target the apparent
provoking receptor. If response is only partially effec-
tive, consider adding new therapy targeting alternate
neurotransmitter pathways, rather than changing the
agent. If a patient presents and is already established
on anti-emetic therapy, apply a second and different
class of anti-emetic to augment and address symptoms
given the mechanistic interplay.
7
Acknowledge major
side effect profiles and drug interactions as there
are many. Fortunately, the role of the EDP is acute
symptom management and many of the long term
drug effects can be scrutinized further once comfort
has been provided.
In this advanced illness population, common pal-
liative causes, associated neurotransmitters and drug
suggestions can be abridged using the AVOMIT
mnemonic (Table 2).
8
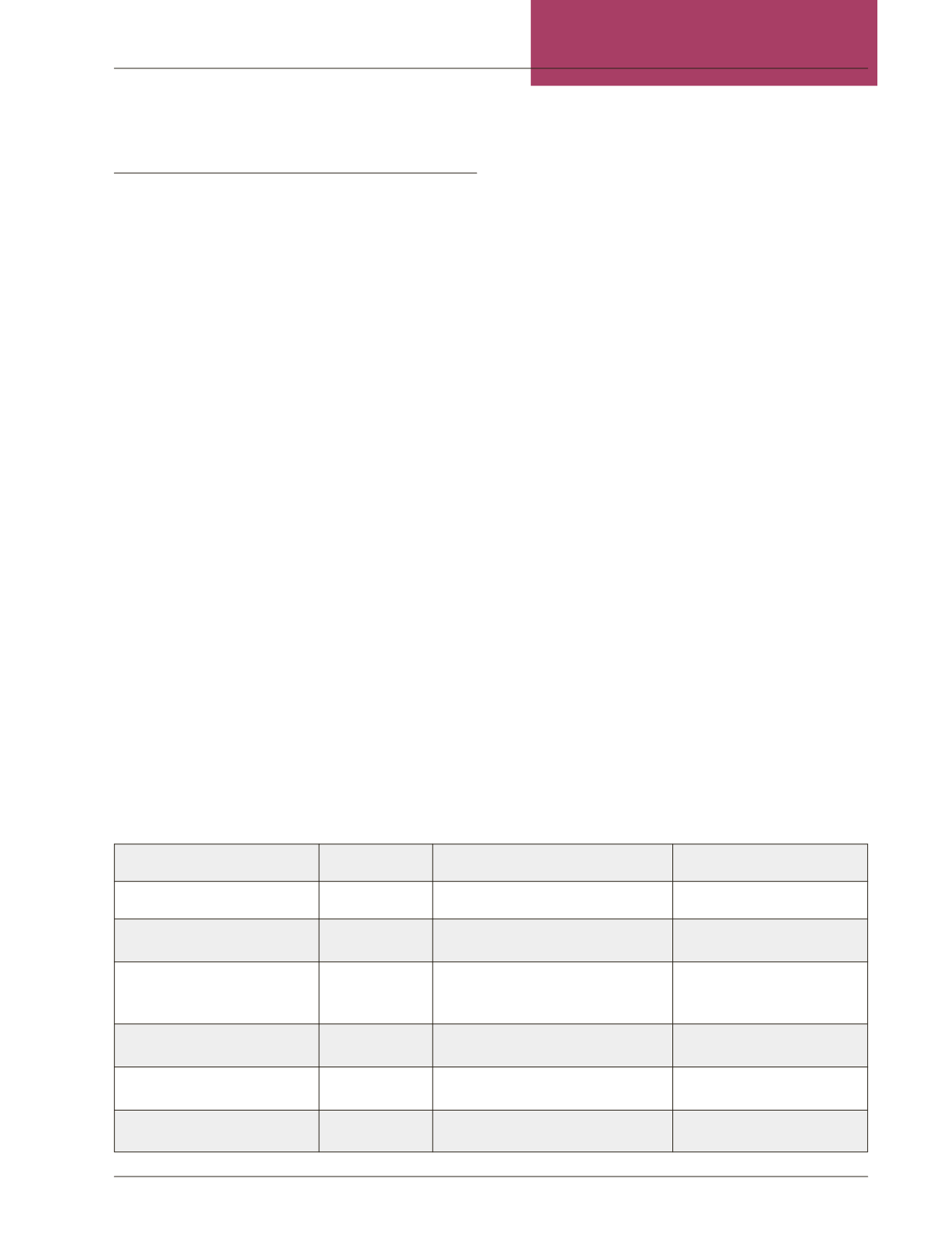
Table 2: Nausea and Vomiting in Palliative Care
Cause
Receptor
Drug
A
nxiety/Anticipate
Central
Benzodiazepines
V
estibular (Meds/Mets)
AcH, H1
Promethazine, Meclizine,
Diphenhydramine
O
bstruction (bowel,
constipation, visceral,
metastases)
AcH, H1,
D2, 5HT3/4
Metoclopramide, Prochlorperazine,
Haldol, ondansetron
Do not use metoclopramide
in complete obstruction
M
edication/Metabolic (CTZ)
D2, 5HT3
Metoclopramide, Haloperidol,
Ondansetron
I
nfection/Inflammation
AcH, H1, 5HT Prochlorperazine, Promethazine,
Ondansetron
T
umor/Toxins
D2, 5HT3
Haloperidol, Metoclopramide,
Ondansetron, Prochlorperazine,
















