
16
Vol. 67, No. 1 2016
Northeast Florida Medicine
DCMS online
. org
Palliative Care
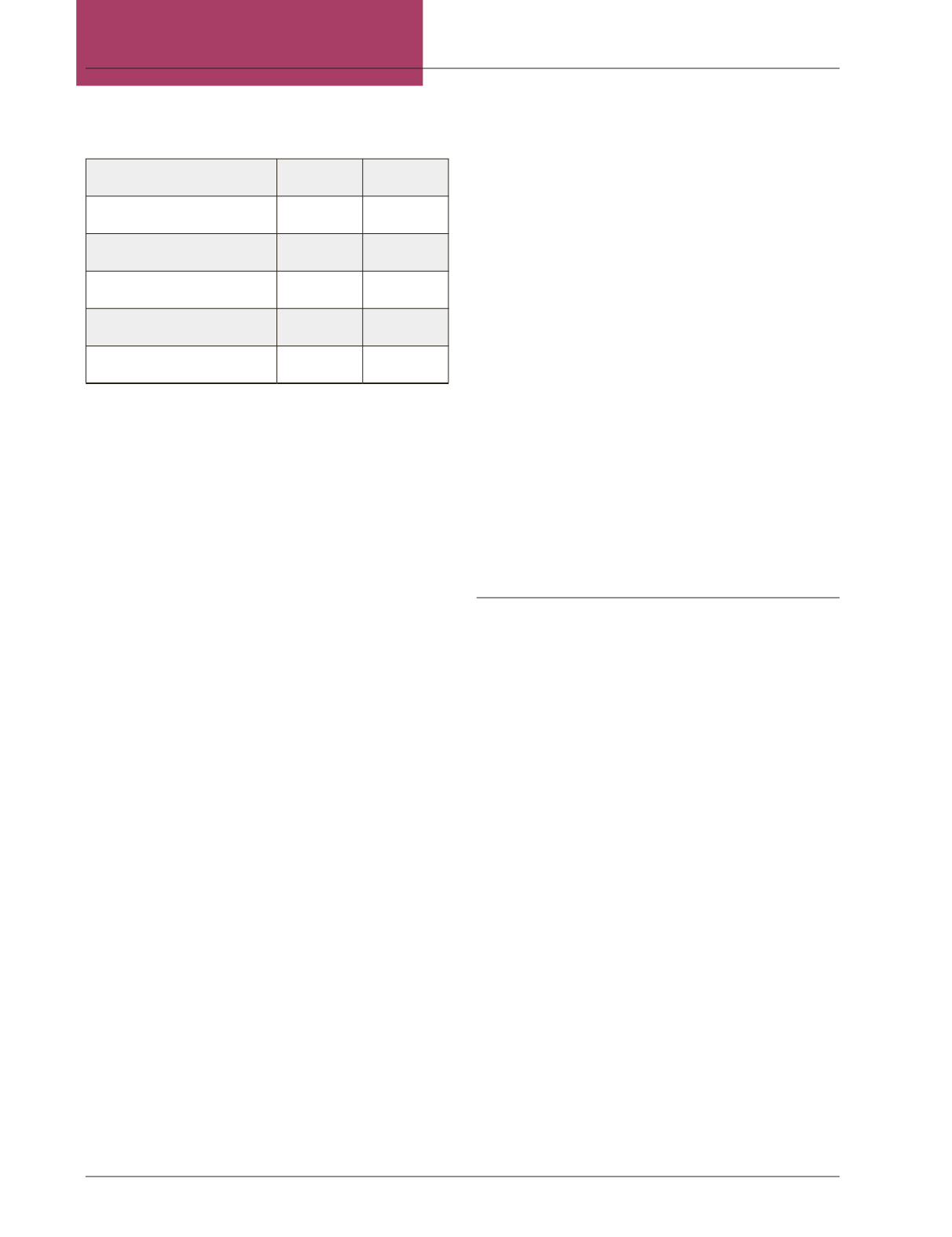
Table 1: Opioid Equianalgesic Dosing
Drug
IV (mg)
PO (mg)
Morphine
10
30
Hydromorphone
1.5
7.5
Oxycodone
~
20
Hydrocodone
~
30
Fentanyl
12- 25mcg
~
Once the etiology of pain has been better understood,
thenext vital step inmanagement shouldbe todetermine
if the patient is opiate naïve or tolerant. In general, if a
patient has been using a total daily dose (TDD) equiv-
alent to 60 mg of oral morphine (30mg oxycodone)
longer than one week, they are to be considered opioid
tolerant and thus will require higher dosing to achieve
therapeutic effect.
2,3
In a naïve patient, morphine is typically the initial
drug of choice at 5-10mg IV, or 0.1mg/kg. The patient
should be reevaluated in 10-15 min and dose escalated
or repeated, if necessary. Detailed titration regimens
exist. However, for simplicity, it is safe to say that
25-50 percent increases would be safe and prudent if
mild to moderate pain persists. If severe, uncontrolled
pain is reported dose escalation of 50-100 percent is
appropriate.
3,4
Sedation would be a noticed side effect
before respiratory depression. Fentanyl should be used
in renal/liver failure patients. The elderly should be
managed more conservatively, typically starting with
half the standard dose.
In the opiate tolerant patient, all chronic opiate med-
ications, long and short acting, should be converted to
theTDDofmorphine equivalents.The initial parenteral
dose should be 10 percent of TDD. Again, the patient
shouldbe reevaluated and redoseduntil adequate control
is achieved. Understand that those on chronic opiates
will require disproportionate dosing to achieve control
compared towhat is needed for their baseline dailyneeds.
This, however, may exceed what seems to be common
practice.
3
At reassessment it is standard to increase your
initial dose 50-100 percent if pain is unchanged or
increasing. If pain remains at a level of 4-6 by patient
report then repeat the same dose. If pain level is at 0-3,
the current treatment is effective.
3
Should respiratory depression become an issue in the
opioid tolerant patient, it is recommended to provide
supportive care, stimulate the patient and wait for drug
metabolism.
3
An IV dose should be at peak effect in
approximately 15 minutes. Administration of naloxone
is discouraged unless acutely necessary as this can reverse
pain control and result in agonizing rebound pain for
the chronically tolerant patient.
Of note, recent literature is supporting lower, non-dis-
sociative use of ketamine in opioid tolerant patients.
5
Ketamine blocks the NMDA receptor and is also a weak
opioid antagonist. A conservative dose of 0.1mg/kg can
be given as an adjuvant to the initial opioid dose. Studies
show that this can greatly reduce overall opiate need and
decrease painperception in suchopioid tolerant patients
enduring acute pain crisis.
5
Dyspnea
Dyspnea or breathlessness is a common subjective
complaint and a leading reason for palliative patients
presenting to the ED. It can provoke great anxiety for
both the patient and caregiver. Dyspnea is a symptom
of totality in that, in addition to its physical effects, it
also influences psychological anxiety and suffering, and
has social implications on those close to the patient.
6
In line with “what can we do,” a search for a reversible
condition should always be sought and addressed. De-
spite definitive intervention, symptom management is
still essential.
After supplemental oxygen, which may or may not
be of benefit unless the patient is hypoxic, opioids are
the drug of choice in managing dyspnea. Doses for the
opioid naïve patient are much lower than those required
for acute pain management.
3,4
Start with morphine
2-5mg IV (5 mg PO) and repeat dose every 15 minutes
titrating to effect or sedation, which will occur prior to
respiratory depression. In the opioid tolerant patient,
doses may be started at 10-25 percent TDD every 30
minutes.
3,4
In renal and liver failure patients, fentanyl
shouldbe used. Additionally, anxiolytics canbe provided
for the anxiety associated with breathlessness; monitor
closely for concomitant sedation.
















