
DCMS online
. org
Northeast Florida Medicine
Vol. 67, No. 1 2016
23
Palliative Care
use a single device to provide higher quality individualized
treatments than the historical standards. This also comes at
a fraction of the cost and with a much smaller investment
in staffing and departmental space needs. Hopefully, the
ability and inherent cost to accurately target and deliver
therapy will plummet as technology advances. In terms of
the biotechnology, radiation therapy continues to pursue
advances in the fields of radiosensitization, radioprotection
and co-targeting of malignant tissues. See Figure 5 as an
example of a modern linear accelerator.
Conclusion
Over the last several decades, radiation therapy has
proven to have a large positive impact upon the quality of
life of oncologic patients requiring palliative interventions.
Moreover, early referral to a palliative care specialist has
demonstrated improved survival and decreased depression
rates while avoiding futile care at the end of life.
38
Joint ef-
forts with palliative care specialists will continue to evaluate
techniques to minimize radiation side effects and improve
outcomes for patients receiving palliative radiotherapy. As
in all studies, the true endpoints will be improving quality
of life and extending median survival.
v
References
1. Jones JA, Lutz ST, Chow E, et al. Palliative radiotherapy
at the end of life: a critical review. CA Cancer J Clin.
2014 Sep-Oct;64(5):296-310.
2. Hartsell WF, Yajnik S. Palliation of Bone Metastases. In:
Perez and Brady’s Principles and Practice of Radiation
Oncology, 6th ed. Philadelphia, Pa: Lippincott Williams
& Wilkins; 2013. p. 1778-1790.
3. Ryu S, Jin R, Jin J, et al. Pain control by image-guided
radiosurgery for solitary spinal metastasis. J Pain Symp-
tom Manage. 2008 Mar;35(3):292-8.
4. Gerszten PC, Burton SA, Ozhasoglu C, Welch WC.
Radiosurgery for spinal metastases: clinical experience
in 500 cases from a single institution. Spine (Phila Pa
1976). 2007 Jan 15;32(2):193-9.
5. Salama JK, Hasselle MD, Chmura SJ, Malik R, et al.
Stereotactic body radiotherapy for multisite extracranial
oligometastases: final report of a dose escalation trial in
patients with 1 to 5 sites of metastatic disease. Cancer.
2012 Jun 1;118(11):2962-70.
6. Niibe Y, Hayakawa K. Oligometastases and oligo-recur-
rence: the new era of cancer therapy. Jpn J Clin Oncol.
2010 Feb;40(2):107-111.
7. Sperduto PW, Chao ST, Sneed PK, et al. Diagno-
sis-specific prognostic factors, indexes, and treatment
outcomes for patients with newly diagnosed brain me-
tastases: a multi-institutional analysis of 4,259 patients.
Int J Radiat Oncol Biol Phys. 2010 Jul 1;77(3):655-61.
8. Patchell RA, Tibbs PA, Walsh JW, et al. A randomized
trial of surgery in the treatment of single metastases to
the brain. N Engl J Med. 1990 Feb 22;322(8):494-500.
9. Andrews DW, Scott CB, Sperduto PW, et al. Whole
brain radiation therapy with or without stereotactic
radiosurgery boost for patients with one to three brain
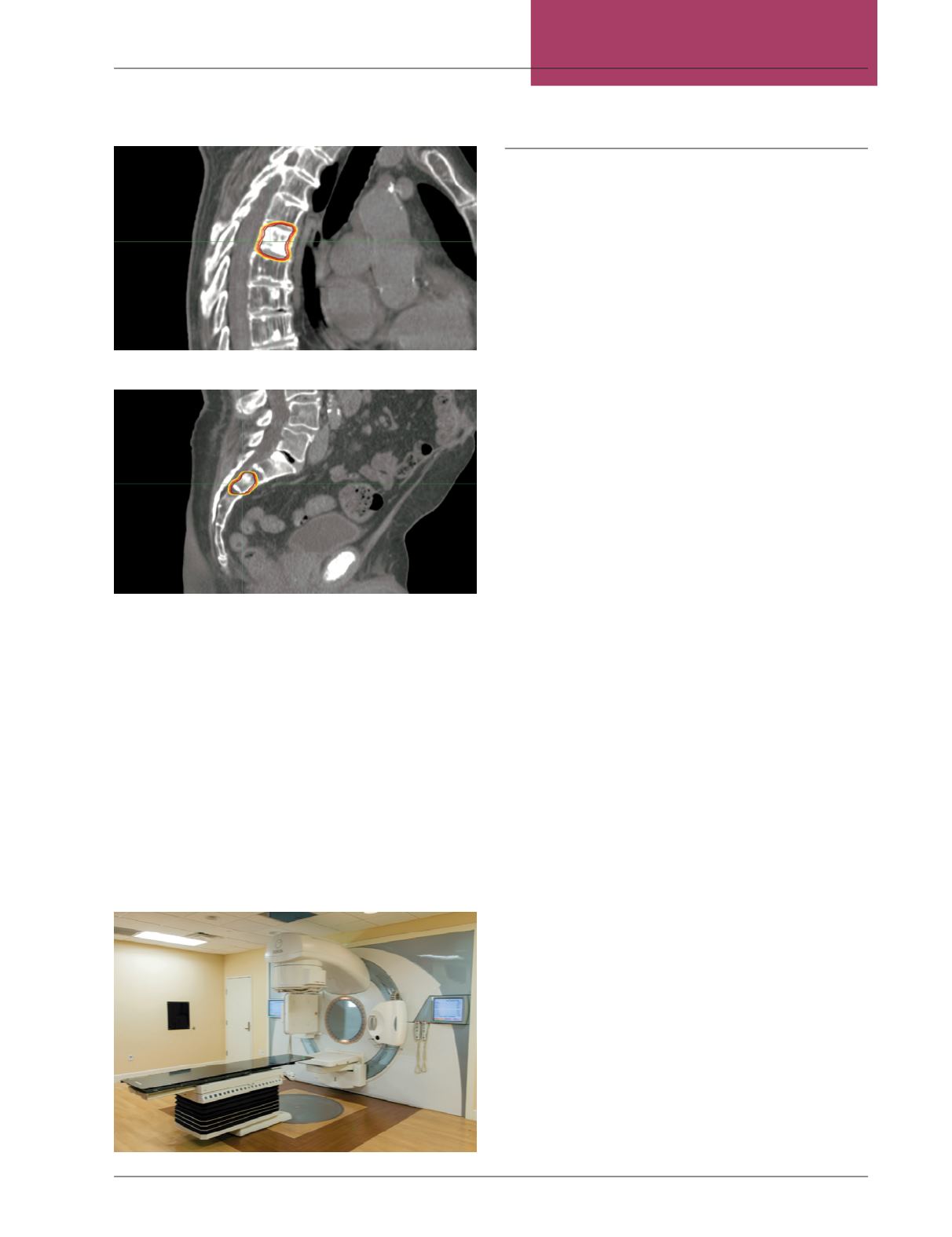
Figure 5:
Modern Linear Accelerator with fully integrated CT Image Guidance
Radiation Therapy (IGRT), Intensity Modulated Radiation Therapy
(IMRT) and Volumetric Modulated Arc Therapy (VMAT).
Figure 3:
Figure 4:
















