
56
Vol. 67, No. 1 2016
Northeast Florida Medicine
DCMS online
. org
Palliative Care
and their families. Often the screening is the responsibility
of other members of the interdisciplinary team.
6
A basic screening can take place in the form of a “getting
to know you” conversation and can be as basic as asking
a few questions such as, “How do you find strength in
difficult situations?” or “In whom or what do you place
your confidence and trust for your overall well-being?”
Other questions might be, “Is there a spiritual compo-
nent for you?” and “Are you part of a particular faith
community?” In addition to asking questions such as
these, paying attention to the questions a patient is asking
is equally, if not more, important. He or she might be
asking, “Why is this happening to me?,” “What did I do
to deserve this?” or questions about God, his/her higher
power or his/her religious tradition. The domains of
suffering, derived from the Oxford Textbook of Palliative
Medicine, (Table 1) can assist in questions one might use
in a basic spiritual assessment.
7
Chronically ill patients
can experience suffering across four domains: physical,
emotional, social and spiritual. Basic screening skills, tools
and techniques, which may include inquiring about hopes
and dreams, fears and concerns and values or beliefs, can
be acquired with nominal effort, are “second nature” for
the majority of palliative care providers and can come from
any member of the interdisciplinary team. The National
Consensus Project for Quality Palliative Care guidelines
state that an assessment is best done when a standardized
instrument, such as the Functional Assessment of Chronic
Illness Therapy-Spiritual Well-Being (FACIT-Sp-12), is
used.
8
(Figure 1)
Another commonly used resource is Dr. Christina
Puchalski’s FICA Spiritual History Tool.
FICA
is an
acronym for a guide to effective questions:
F
aith or
beliefs (“What do you believe in that gives meaning to
your life?”),
I
mportance and influence (“How important
is your faith to you?”),
C
ommunity (“Are you a part of
a religious or spiritual community?”), and
A
ddress or
A
pplication (“How would you like us to address these
issues in your health care?”).
9
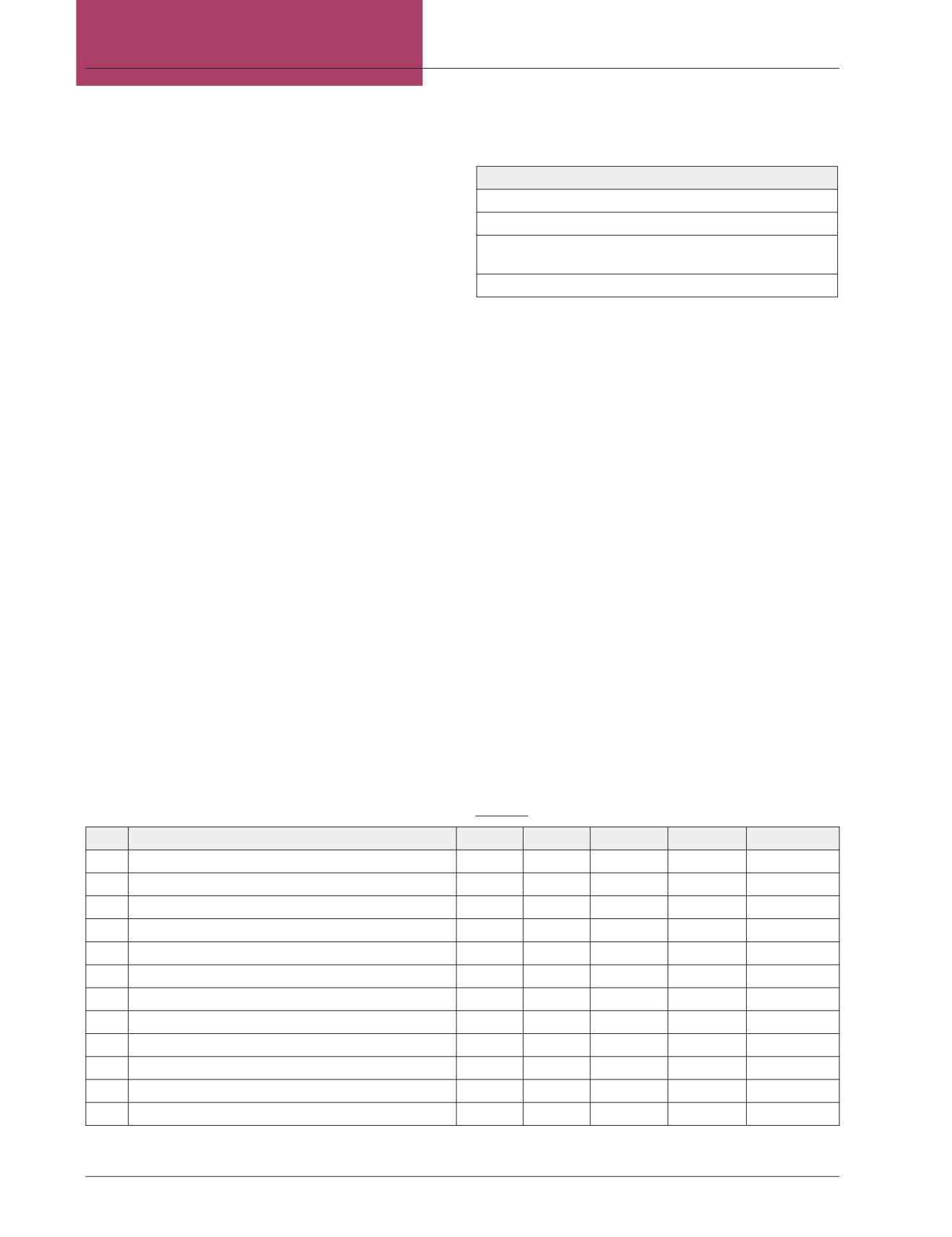
FACIT-Sp-12: Functional Assessment of Chronic Illness Therapy - Spiritual Well-Being; The 12-item Spiritual Well-Being Scale
8
Below is a list of statements that other people with your illness have said are important.
Please circle or mark one number per line to indicate your response as it applies to the past 7 days.
Not at all A little bit Some-what Quite a bit Very much
Sp1
I feel peaceful
0
1
2
3
4
Sp2
I have a reason for living
0
1
2
3
4
Sp3
My life has been productive
0
1
2
3
4
Sp4
I have trouble feeling peace of mind
0
1
2
3
4
Sp5
I feel a sense of purpose in my life
0
1
2
3
4
Sp6
I am able to reach down deep into myself for comfort
0
1
2
3
4
Sp7
I feel a sense of harmony within myself
0
1
2
3
4
Sp8
My life lacks meaning and purpose
0
1
2
3
4
Sp9
I find comfort in my faith or spiritual beliefs
0
1
2
3
4
Sp10
I find strength in my faith or spiritual beliefs
0
1
2
3
4
Sp11
My illness has strengthened my faith or spiritual beliefs
0
1
2
3
4
Sp12
Iknowthatwhateverhappenswithmyillness,thingswillbeokay
0
1
2
3
4
Permission to use the FACIT-Sp-12 is required and is available at
FACIT.org.
Figure 1:
Domains of Suffering/Concept of Total Pain
7
PHYSICAL –
What
– e.g. pain, nausea, dyspnea, fatigue
EMOTIONAL –
How
– e.g. angry, depressed, confused, anxious
SOCIAL –
Who
– e.g. relationships, family/friend conflict and
support
SPIRITUAL–
Why
– e.g. attributingmeaning toundesired events
Adapted from: Cherny N, Fallon M, Kaasa S, et al. Oxford Textbook of Palliative
Medicine. 5th ed. Oxford: Oxford University Press; 2015.
Table 1:
















