
DCMS online
. org
Northeast Florida Medicine
Vol. 67, No. 1 2016
47
CME
IV. The Batterer
An abuser may lead what appears to be a “normal” life
outside the home. He/she can be a productive member of
society and the violent behavior may only occur behind
closed doors. The abuser may have been a victim of abuse
as a child. Men who lived in violent homes as children are
more likely to be violent with their adult partners than
men who were reared in non-violent homes.
24
For the
batterer, casting blame and guilt on the victim can elevate
their own sense of worth. Like victims of IPV, batterers
also are often abusers of alcohol and drugs.
Clinical Presentation
A patient experiencing intimate partner violence may
present in a variety of manners. Often they present with
inconsistent injuries or vague explanations of injuries.
Victims may also have poor follow- up, frequently miss
appointments, be non-compliant with medications or
may be reluctant to comply with a physical examination.
Their partner may be present and reluctant to leave the
room during history or examination. It is estimated
that between two and seven percent of acute emergency
room visits are from IPV.
30
Often victims will seek care
in the emergency department because they are likely to
see different healthcare providers each time and there is
less follow-up. The patient’s social history may include
substance abuse disorders, tobacco abuse, anxiety and
depression. Higher rates of previous abuse as a child
and suicide attempts are also observed.
30-32
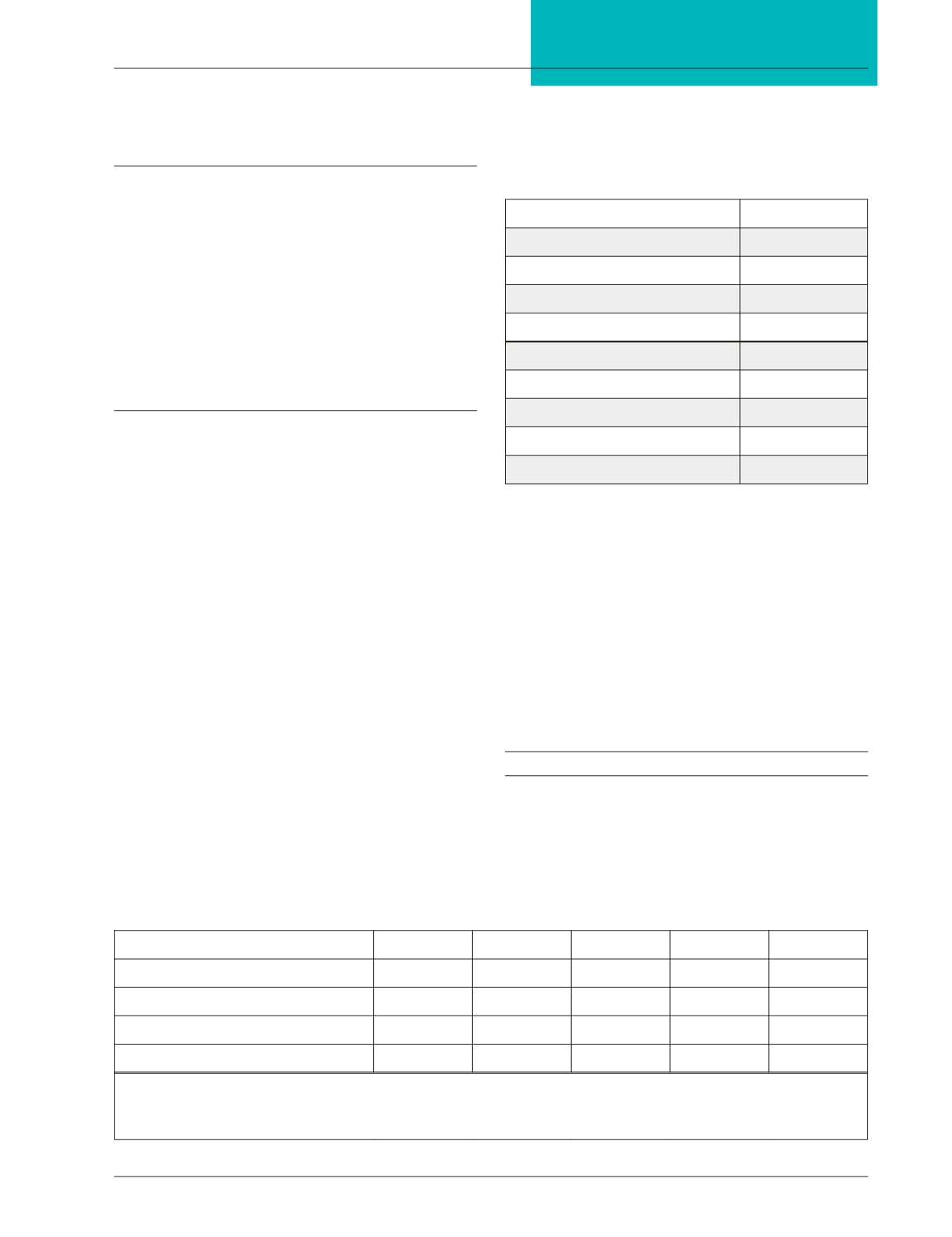
According to
Medical and Psychosocial Diagnoses in Women with a
History of Intimate Partner Violence, published in 2009,
several signs and symptoms are associated with intimate
partner violence and are noted in Figure 2. Signs and
symptoms with the highest relative risk include anxiety,
substance abuse, tobacco abuse, depression, headache,
sexually transmitted infections, contusions/abrasions, low
back pain and lacerations (Figure 2).
33
Persons suffering
from IPV and/or sexual/physical abuse also have a 1.5 to
2 times greater risk of having functional gastrointestinal
symptoms.
30
Victims of intimate partner violence also
reported worse physical and mental health and increased
chronic pain and disability preventing employment.
Physical examination is often unremarkable. However,
the physician may discover old fractures, cigarette burns
or bites in areas that are not readily visible.
The Role of the Healthcare Provider:
Screening
All health care providers should remain alert for the
presence of IPV, even in asymptomatic patients. The
United States Preventive Services Task Force states that
Table 2:
The HITS Screening Tool for Domestic Violence
How Often Does Your Partner
Never
Rarely
Sometimes
Fairly Often Frequently
Physically hurt you
1
2
3
4
5
Insult or talk down to you
1
2
3
4
5
Threaten you with harm
1
2
3
4
5
Scream or curse at you
1
2
3
4
5
A total score of more than 10 is suggestive of intimate partner violence.
The New England Journal of Medicine. 2012-11; 367:2071-2073.
Figure 2:
Common Presenting Symptoms
in Victims of Intimate Partner Violence
Signs/symptoms associated with IPV Relative Risk Ratio
Substance Abuse
6.33
STDs
3.30
Depression
3.24
Anxiety
2.73
Tobacco Abuse
2.34
Lacerations
2.15
Contussions/abrassions
1.72
LBP
1.58
Headache
1.56
















