40
Vol. 67, No. 1 2016
Northeast Florida Medicine
DCMS online
. org
Palliative Care
Case Three:
Rev. & Mrs. M. were new primary care pa-
tients with the intent to prepare the Reverend to transition
into hospice. His functional capacity was relatively high
(Karnofsky Score of 50). (Table 2) His wife, with a FAST
dementia score of 6 (Impaired Activities of Daily Living
with incontinence), was lovingly attended to by her son and
daughter-in-law and grandchildren. However, suddenly and
unexpectedly she required significant medical attention for
acute respiratory distress. Over several days her condition
worsened. Her other visiting children came specifically
for a family meeting to consider options, including in-
tubation. Interestingly, the family members interpreted
their father’s Lutheran biblical scripture in diametrically
opposing manners; half of the family members requested
that “nature prevail to a natural death” and the other half
requested that “every God-givenmedical treatment” be ren-
dered. The family conference, mediated by the consultant,
created a single time-limited trial, which was acceptable
to all, allowing her to survive.
Negotiating a compromise with a time-limited trial is
an invaluable “win-win” strategy that allows everyone to
know their perspectives were honored. Ultimately, when
the next medical urgency presented itself, no attempts at
resuscitation and all manner of comfort measures were
rendered. Anticipatory grief counsel was provided to the
husband and the family. The authors admit that “grief is
grief ”; however, preparation for “what might happen” may
mitigate suffering by the survivors too.
10 Things Palliative Care Clinicians Wished
Everyone Knew About Palliative Care:
Please consider these pearls of palliative wisdom from a
recent publication by experts in palliative medicine; the au-
thors recommend this list of theTop 10Things Palliative Care
Clinicians Wished Everyone Knew About Palliative Care:
7
1. Palliative care can help address the multifaceted aspects
of care for patients facing a serious illness.
2. Palliative care is appropriate at any stage of serious illness.
3. Early integration of palliative care is becoming the new
standard of care for patients with advanced cancer.
4. Moving beyond cancer: Palliative care can be benefi-
cial for many chronic diseases. This includes non-curable
non-cancer medical conditions such as end stage renal, liver,
heart, lung failure, as well as various neurological diseases.
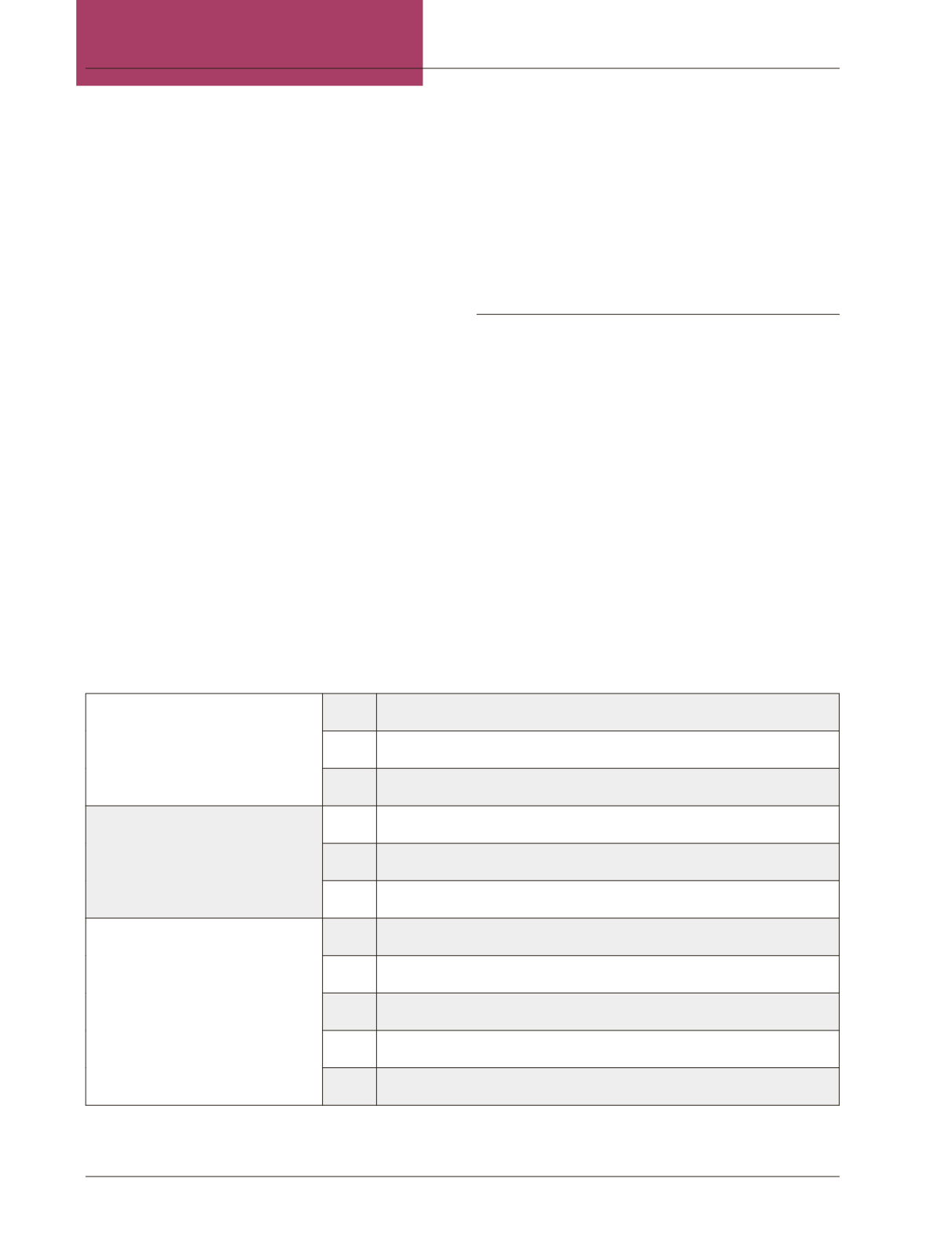
Table 2:
Karnofsky Performance Status Scale Definitions Rating (%) Criteria
7,12
Able to carry on normal activity and
to work; no special care needed.
100
Normal no complaints; no evidence of disease.
90
Able to carry on normal activity; minor signs or symptoms of disease.
80
Normal activity with effort; some signs or symptoms of disease.
Unable to work; able to live at home and
care for most personal needs; varying
amount of assistance needed.
70
Cares for self; unable to carry on normal activity or to do active work.
60
Requires occasional assistance, but is able to care for most of his personal needs.
50
Requires considerable assistance and frequent medical care.
Unable to care for self; requires equiv-
alent of institutional or hospital care;
disease may be progressing rapidly.
40
Disabled; requires special care and assistance.
30
Severely disabled; hospital admission is indicated although death not imminent.
20
Very sick; hospital admission necessary; active supportive treatment necessary.
10
Moribund; fatal processes progressing rapidly.
0
Dead
The Karnofsky Performance Scale Index allows patients to be classified as to their functional impairment. This can be used to compare ef-
fectiveness of different therapies and to assess the prognosis in individual patients. The lower the Karnofsky score, the worse the survival for
most serious illnesses. The assessment is named after Dr. David A. Karnofsky, who described the scale with Dr Joseph H. Burchenal in 1949.
















