
30
Vol. 67, No. 1 2016
Northeast Florida Medicine
DCMS online
. org
CME
and family members indicated a high level of interest and
engagement in the discussions and likewise indicated a desire
to share their positive experiences with others.
Lessons learned from the pilot sites
While the health system/hospital partners were pleased
with the results, they noted that lessons learned from the
pilots will help further develop ACP in the community.
Outpatient sites, such as physician offices, are ideal locations
for the introduction of ACP, recruitment strategies and
initiating the conversation. Consistency in site leaders and
facilitators is also important for the success of implemen-
tation and expansion. As facilitators became more skilled
through practice, the length of time they spent in individual
conversations decreased. Resource needs were identified for
scalability in the hospitals. Facilitator turnover impacted
patient/participant volume, as some sites had not prepared
for this possibility. On occasion, when patients/participants
left the conversation with an incomplete document, they
never completed or returned it, as teams had not created a
follow-up process.
Although pilot partners exceeded program goals in various
measures, expectationswere higher, leading to teamleadership
and facilitator disappointment. Although no completion goal
was established prior to implementation, the pilot partners
did not believe that an appropriate number of advance di-
rective documents were completed. They expressed concern
that quality ACP conversations take too much time and
dissemination and spread throughout an organization can
be a complex, time-consuming process. Respecting Choices®
leadershipvalidated that these are commonconcerns expressed
by teams following an initial implementation. They verified
that program success is not judged by the number of complet-
ed documents, but instead at the organizational level. They
also helped the teams develop questions to address in future
implementations to measure success:
1) Has a process been designed so that targeted patients
can be routinely approached and ACP initiated?
2) If patients express an interest in ACP conversations,
can they be connected to a qualified ACP facilitator?
3) If and when an advance directive is created, can it be
reliably made part of the patient’s medical record?
4) Has a standardized advance directive document been
designed, tested and disseminated?
5) Have standardized ACP patient education and en-
gagement materials been developed and tested?
6) Are outcomes being monitored and reported regularly?
7) Is the oversight committee developing an overall
community engagement and outreach strategy?
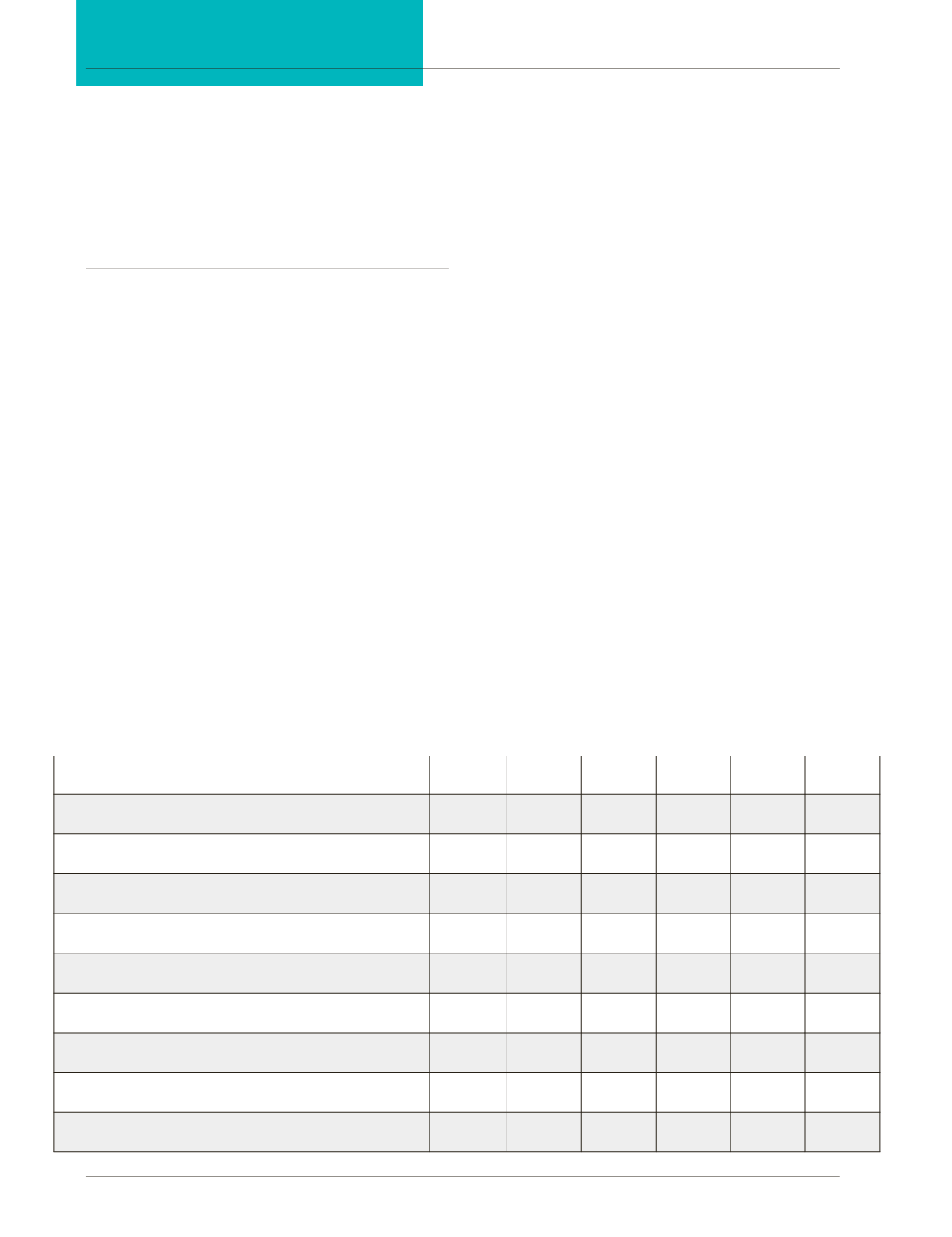
NE Florida
La Crosse
WI Region All Florida
National
Average 90th %ile 50th %ile 10th %ile
Hospital admits per 1,000 decedents
during the last 6 months of life
1387.16
1063.6
1420.3
1336.5
1506.9
1300.9
1066.9
Inpatient days per decedent during
hospitalization in which death occurred
1.27
0.94
1.35
1.52
1.96
1.34
0.91
Inpatient days per decedent during
the last 6 months of life
9.54
5.3
9.7
8.7
10.1
8.2
6.0
Inpatient spending per decedent during the
hospitalization in which death occurred
3267
2541
3387
4171
5729
3541
2659
Inpatient spending per decedent during
the last 6 months of life
14,553
11,175
15,805
16,243
20,749
14,154
11,864
Percentage of decedents admitted to ICU/CCU
during the hospital stay in which death occurred
14.9% 9.2% 15.1% 15.4% 18.6% 14.5% 10.7%
Percentage of decedents spending 7 or more days in
ICU/CCU during the last 6 months of life
21.2% 2.7% 21.7% 14.7% 20.6% 13.0% 6.4%
Percentage of deaths occurring in hospital
21.2% 19.1% 18.8% 22.1% 26.4% 21.5% 16.3%
Percentage of decedents hospitalized at least
once during the last 6 months of life
70.2% 60.6% 70.9% 68.3% 72.8% 67.9% 60.7%
Figure 1:
















