
DCMS online
. org
Northeast Florida Medicine
Vol. 66, No. 4 2015
43
Inflammatory Bowel Disease
may also be seen in rheumatoid arthritis and certain hemato-
logic malignancies. It appears that immunological factors and
neutrophil dysfunctionmay play a role in its evolution. Classic
pyoderma begins as a pustule or vesicle but then ruptures,
becomes necrotic, and progresses to ulceration in several days.
The lesion is extremely painful. These lesions tend to have a
predilection for the lower extremities, but may occur adjacent
to stomas or even on the genitalia. The patient may be system-
ically ill with fever, malaise, arthralgias, and myalgias. These
ulcerationsareinfiltratedbyinflammatorycellswhicharemostly
neutrophils. The differential with PG includes infections, ma-
lignancies, vasculitides, venous stasis ulceration, and peripheral
vascular disease. Skin biopsy may be helpful in excluding other
conditions if inflammatory bowel disease is not lurking.
Without treatment, PG can last for years. Systemic
steroids are first line therapy for PG and usually create a
rapid response. On occasion, certain immune modulating
treatment such as Dapsone, cyclosporin, mycophenolate,
topical tacrolimus, or even intravenous immunoglobulins
may be needed. Infliximab and adalimumab are clearly
first line therapies. At times, aggressive debridement by a
skilled surgeon with grafting may be needed. Hyperbaric
oxygen may be of benefit. Antibiotics play no specific role
in treating these lesions unless secondarily infected. Plas-
mapheresis has been employed for refractory PG. Overall,
the treatment of the underlying inflammatory bowel disease
allows these lesions to slowly heal. An atrophic scar may be
left, and it is not unusual for it to take weeks or months
to clear. Sweet’s syndrome is characterized by tender, red,
inflammatory nodules or papules that usually affect the
upper limbs, face, or neck. It is in the group of acute neu-
trophilic dermopathies similar to pyoderma gangrenosum.
This lesion has a strong predilection for women and mostly
is seen in patients with colonic disease. As a rule, the rash
is associated with active IBD disease, but may also precede
the onset of intestinal symptoms and up to 21 percent of
patients with eventual inflammatory bowel disease.
7,8
Ocular Manifestations
Awide range of ocular manifestations have been recorded
in patients with IBD. These complications are commonly
associated with joint complaints as well. The incidence
varies from 4-12 percent in both UC and CD, although
uveitis and iritis are more commonly seen in patients with
UC, and episcleritis more commonly in Crohn’s disease.
9
Episcleritis is a painless red eye characterized by hyperemia
of the sclera and conjunctiva with itching and burning. As
a rule, this disorder does not require a specific treatment
other than the underlying disease activity that is treated. It
will respond to topical steroids.
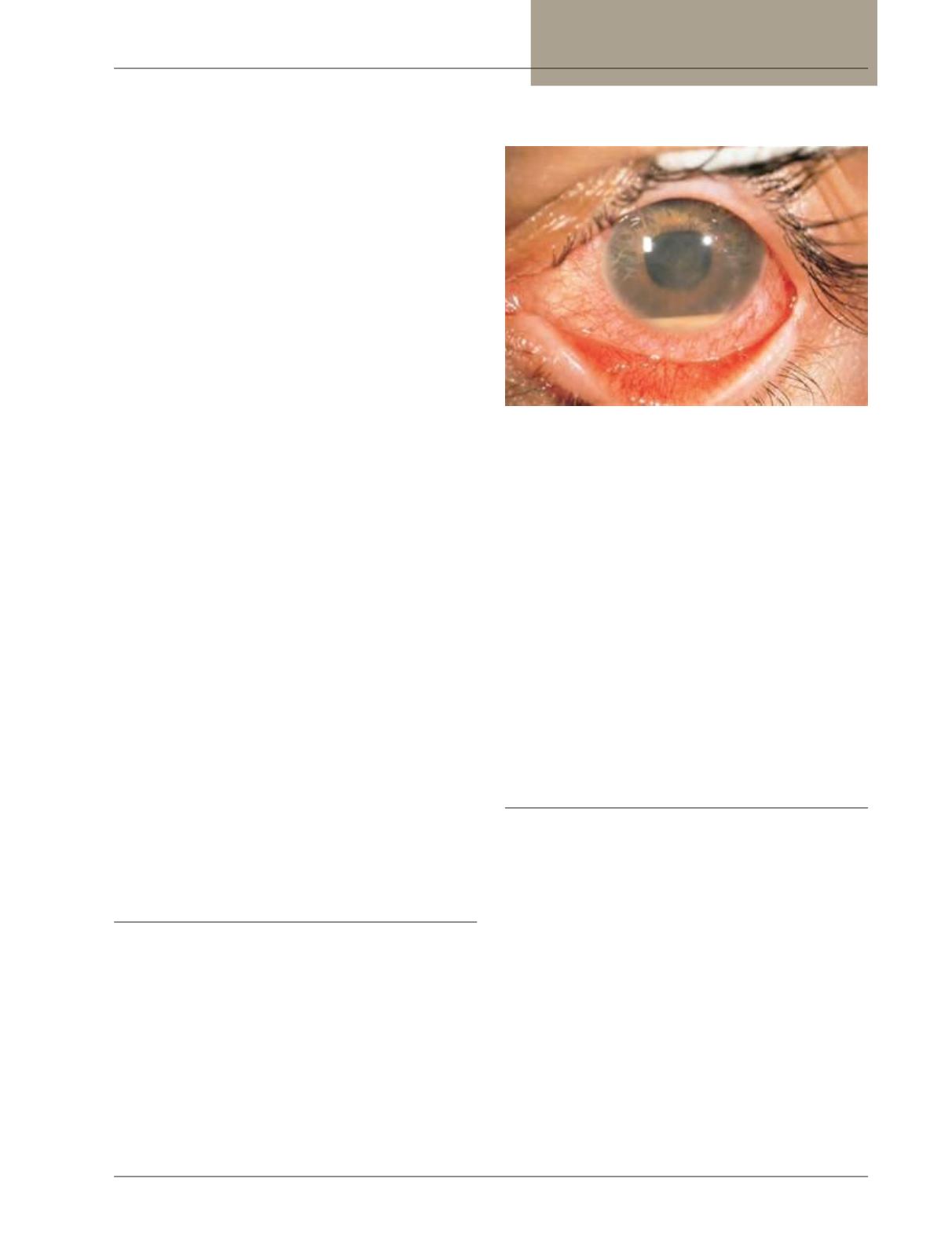
Figure 4:
Uveitis with hypopyon (Crohn’s)
Uveitis is less common (around 2-3 percent of patients),
but has potentially severe consequences.
9
(Figure 4) It is
often associated with UC, and is commonly bilateral in a
long lasting condition. Patients have eye pain, blurred vision,
photophobia, and severe headaches. Progression to loss of
vision can occur, and these patients need to be seen by an
ophthalmologist quickly. Slit lamp exam will confirm the
diagnosis. Uveitis is treated with steroids both systemically
and topically, and the ophthalmologist should be actively
involved in care of this condition. In addition, there has
been tremendous success with the use of infliximab in this
disorder.There is a high prevalence of p-ANCA (perinuclear
anti-neutrophil cytoplasmic antibodies) in patients with
UC that have uveitis.
9
This is also seen in patients with
sclerosing cholangitis and erythema nodosum.
Hepatobiliary Disease
It is estimated that 5-15 percent of patients with inflam-
matory bowel disease will develop some form of hepatobi-
liary disease. Now, with sophisticated magnetic resonance
cholangiopancreatography (MRCP), that prevalence may
be understated. Primary sclerosing cholangitis (PSC) consti-
tutes the most important condition relatively specific to the
underlying IBD. This disease has an unknown etiology, has
no proven effective treatment, and liver transplantation is the
only way of extending a patients’ life expectancy. Patients can
also develop pericholangitis, steatosis, a nonspecific chronic
hepatitis, cryptogenic cirrhosis, and cholelithiasis. PSC is a
chronic cholestatic disease characterizedby progressive inflam-
mationof the intrahepatic and extrahepatic bile ducts followed
by fibrosis and, in its worst case, biliary cirrhosis with liver
failure. 70 percent of victims are male, most are HLA-DR3,
B8 positive, and up to 75 percent of them will have IBD.
10
Cholangiocarcinoma may also develop within this spectrum.
















